Table of Contents
Menopause and Joint Pain – The Link
When thinking of menopause, most people think of hot flashes and sleepless nights. But have you also noticed more pain in your joints since going into menopause?
Joint point pain during menopause affects more than 50% of women. This is related to the decrease of the active form of estrogen called estradiol. Estradiol has anti-inflammatory properties and helps prevent bone and muscle loss. As you age, your estrogen naturally drops. This leads to the new aches and pains you may have noticed.
Will It Go Away?
Whether your menopausal joint pain disappear depends on various factors, including:
- Activity level
- Diet
- Pain tolerance
We will discuss some different options for how to treat your menopausal joint pain. These can help shorten the length of time and decrease the severity of your symptoms. As always, you should talk to your doctor if you have worsening joint pain that is not improving.
As always, you should talk to your doctor if you have worsening joint pain that is not improving.
Book a Consultation with Dr. Pamela Mehta, MD
The Best Orthopedic Surgeon in San Jose
Dr. Mehta is a board-certified orthopedic surgeon who can help you recover from your joint condition. If you:
- Are Suffering From Pain and Mobility Issues
- Need Orthopedic Assessment and Advice
- Want Treatment From a Top Orthopedic Doctor
We Can Help
Symptoms of Menopausal Joint Pain
There are many different causes of joint pain in menopause. Examples include various types of arthritis, such as osteoarthritis or rheumatoid arthritis. Other causes include pain from weak bones that can result in fractures. If the muscles surrounding the joints are weak you may feel pain in the joint. This is because the joint has more weight than it can carry.
Some types of menopausal joint pain are idiopathic. This means we do not know what causes the pain. Certain symptoms should prompt further investigation by your doctor.
Conditions and their associated symptoms that should prompt you to see a doctor:
| Condition | Symptoms |
| Osteoarthritis: A common disease that affects people as they age, which can become more common during menopause due to hormonal changes. | · Sore joints that swell · Joint pain that is worse in the morning but improves with use (<30 min) · Grating sensation in the joint · Joint weakness or giving out sensation |
| Rheumatoid arthritis: An inflammatory arthritis condition that is most diagnosed from ages 40-60. | · Joint swelling and stiffness that is worse in the morning (>30 min) · Fatigue and decreased appetite · Nodules on hands |
| Fibromyalgia: A chronic condition characterized by widespread pain throughout the musculoskeletal system. The cause is unknown, but it is thought the be due to a combination of factors, including hormones. | · Widespread pain generally in the muscles, ligaments or tendons · Tender points typically around large joints (shoulders, hips, knees) · Fatigue and sleep disturbances |
| Osteoporosis: A condition of weakened bones that are more susceptible to fracture. | · Pain in the spine, wrist, and hips from fractures · Bone tenderness |
Hip Pain During Menopause
Some women have pain only in their hips and are wondering what this could be. Various conditions that can cause hip pain during menopause.
- Hip Bursitis: Inflammation of the bursa, a small, fluid-filled sac that acts as a cushion for the hip joint.
- Hip Tendonitis: Inflammation of the tendon around the hip joint. The tendon connects the joint to the muscle.
- Hip Osteoarthritis: Degeneration of the cartilage or “cushion” of the hip joint.
These conditions have similar symptoms of joint pain, tenderness, and swelling. If you think you may have one of these conditions, it is best to be evaluated by your doctor. Your doctor can help distinguish between these conditions.

How to Treat Menopause and Joint Pain
Do you think you have menopause joint pain? If so, you may be wondering how you can treat it. There are many different options that can provide relief.
Lifestyle changes, such as:
- Exercises
- Dietary changes
- Weight loss
- Stopping substance use
These “lifestyle modifications” or changes can help you feel better. Other treatments include medications, surgery, and supplementation. We will review several of them to help you find the best option for you.

Exercise
Exercise is one of the best treatments for menopause and joint pain. Exercise helps strengthen muscles that support the joints and provide lubrication. Exercise also clears out cellular debris by increasing synovial fluid within the joint. Exercise even releases endogenous or natural opioids that decrease pain sensations.
You may be wondering what type of exercise is best for menopausal joint pain. The answer is resistance training. Resistance training is any exercise where your muscles must overcome some oppositional force. This strengthens the muscles and protects the joints from carrying extra weight.
Examples of resistance training include:
- Body weight squats: Works the chest, shoulders, and knees.
- Lunges: Targets the legs and glutes. Adding weights can increase resistance.
- Push-ups: Strengthen the chest, shoulders, and triceps. You can modify by doing them on your knees.
- Dumbbell rows: Focuses on the back and arms.
- Deadlifts: Great for lower back, glutes, and hamstrings. Work on form then add heavier weights.
- Overhead press: Build shoulder and arm strength. You can use dumbbells or barbell.
- Leg press: Targets the legs and glutes. You can do these on a leg press machine at the gym.

Diet
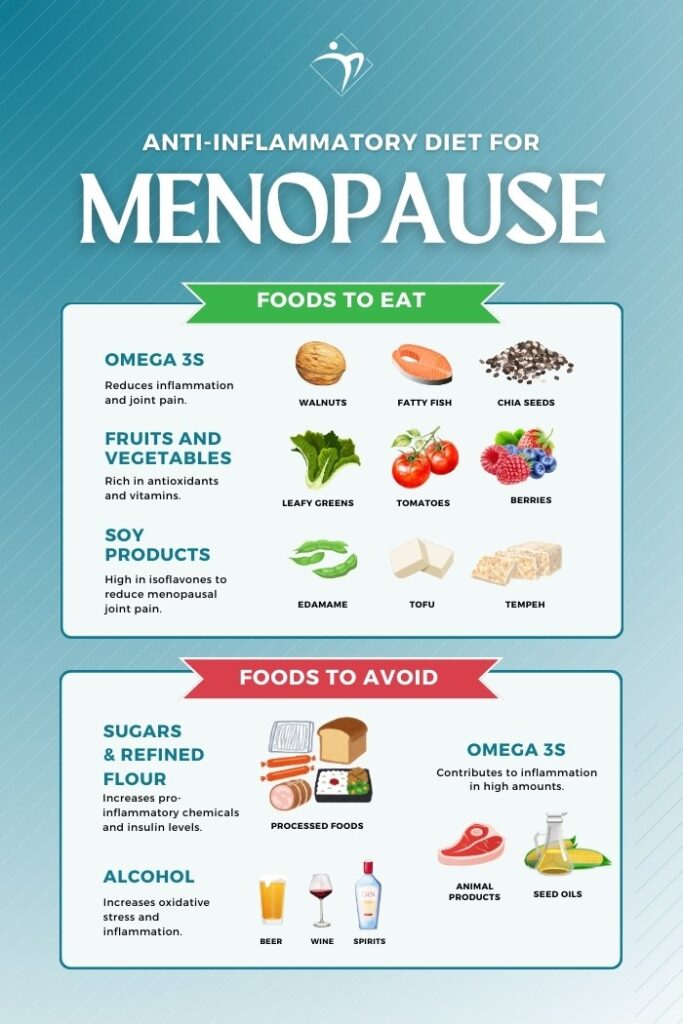
Estrogen falls in menopause can contribute to inflammation. One of the best ways to decrease inflammation is through your diet.
Here are some anti-inflammatory options for your diet:
Omega 3s: Fatty fish, chia seeds, and walnuts. These foods are rich in Omega-3s. This reduces inflammation and joint pain.
Fruits and Vegetables: Berries are rich in antioxidants. Antioxidants help prevent tissue damage and inflammation. Vegetables are full of vitamins and other anti-inflammatory compounds. Examples include leafy greens vegetables, tomatoes, and bell peppers.
Soy products: Edamame, tofu, and tempeh are all foods high in isoflavones. These mimic estrogen and may reduce menopausal joint pain symptoms.
Avoiding the following food groups helps lower inflammation:
Saturated fats: Fats typically found in animal products and seed oils. They contribute to inflammation in high amounts.
Sugars and refined flours: Found in processed foods, they increase pro-inflammatory chemicals. This leads to a higher level of the hormone insulin which increases inflammation.
Alcohol: Alcohol leads to increased oxidative stress and inflammation.
Stop Smoking
Stopping smoking is one of the best things you can do for your general health. Less smoke exposure will help build your bone strength and decrease inflammation.
Weight Loss
Weight loss is one of the best things you can do for your joint pain. Patients with knee pain saw increased function and decreased pain with a 10% weight loss. Other benefits included better mobility, physical health, and mental health.
Combining diet changes with exercise increases the amount of weight loss achievable. Several medications can also help with weight loss.
Are there medications I can use?
There are several types of medications you can use. These include prescription and nonprescription options.
Here are some examples of over-the-counter medications:
- Ibuprofen or other NSAID (or Non-Steroidal Anti Inflammatory Drug)
- Tylenol
- Voltaren (a topical version of NSAIDs)
It is important to know that ibuprofen can affect your kidneys and increase your blood pressure. Tylenol can affect your liver. Talk with your doctor before starting these medications.
Hormone replacement therapy
As you age, your reproductive hormones, estrogen, and progesterone fall. Leading to many of the symptoms of menopause. These include fatigue, weight gain, hot flashes, and yes, even joint pain.
Women who are on hormone replacement therapy (or HRT) tend to report less pain compared to women who are not on HRT.
Before starting this treatment it is best to talk with your doctor to review your health history. If you have a history of blood clots or cancer HRT may not be a good fit for you.
Joint Injections
Injections involve injecting a numbing medicine and a steroid into the joint. This decreases inflammation. 75% of patients have reflief from hip and knee pain injections. If you experience symptom relief you can often get these injections every 3-4 months.
Ready to Recover?
Take the first step in getting back to your normal self, and book an appointment with Dr. Mehta today.
We’re ready when you are!
Is Surgery an Option for Me?
It is possible that surgery may be a good option for you. There are several surgical options depending on the cause of your joint pain.
One option is ligament replacements (ACL or MCL) if you have an injury within the ligament itself. Osteotomy is a type of surgery that helps redistribute the weight in the joint. Joint replacement, such as a knee or hip replacement, can ease the most severe pain from arthritis.
Is surgery a good option for you? You should schedule an appointment with an orthopedic surgeon to discuss.
Are There Non-prescription Options for Me?
Heat and Ice
Heat and ice can reduce sore joints during menopause. Ice packs work well for swollen, hot joints. Heat (heating pad or rice sock) is a great option for stiffness in the joint.
Physical Therapy
Physical therapy works by helping you strengthen the muscles around your joints. This offloads the joint and improves pain. Physical therapists are also qualified to help you with balance. Balance is important in preventing falls later in life.

Vitamins, Supplements, and Natural Remedies
Are you looking for more natural options? You may be wondering what vitamins and supplements are good for menopause and joint pain. Studies have shown several options that may be natural remedies.
- One review found that the following seven supplements decreased joint pain:
- Curcuma longa extract (turmeric/curcumin)
- Collagen hydrolysate
- Passion fruit peel extract
- Boswellia
- Pycnogenol
- L-carnitine
- SAMe is a natural compound in the body that decreases inflammation and stimulates cartilage growth. One study found that SAMe performs as well over time as Celecoxib (an NSAID) in reducing joint pain.
- Resveratrol is an antioxidant found in red grapes and other plants. One study showed that 75mg twice daily improved symptoms of menopause and joint pain.
- Basal oil appears to be a topical option that gives similar relief to diclofenac gel.